COVID-19 mRNA Vaccine Long-Term Immunity: Why Antibody Protection Fades Quickly
COVID-19 mRNA vaccine long-term immunity is limited due to the failure of plasma cells to establish in the bone marrow, leading to a rapid decline in antibodies. Learn why improving vaccine durability is crucial.
The COVID-19 pandemic has seen unprecedented global vaccination efforts, with mRNA vaccines playing a pivotal role in reducing severe illness and deaths. However, concerns have arisen over the longevity of the immunity these vaccines provide. COVID-19 mRNA vaccine long-term immunity has been questioned as studies reveal that while initial protection is strong, it fades much quicker than expected, especially in terms of preventing reinfections and breakthrough cases.
A recent study published in Nature Medicine sheds light on why COVID-19 mRNA vaccine long-term immunity does not last as long as desired. Researchers have found that, unlike vaccines for diseases like tetanus and influenza, COVID-19 vaccines do not establish long-lived plasma cells (LLPCs) in the bone marrow. LLPCs are responsible for producing antibodies over a long period, and their absence explains why COVID-19 antibody levels drop quickly after vaccination.
How mRNA Vaccines Work
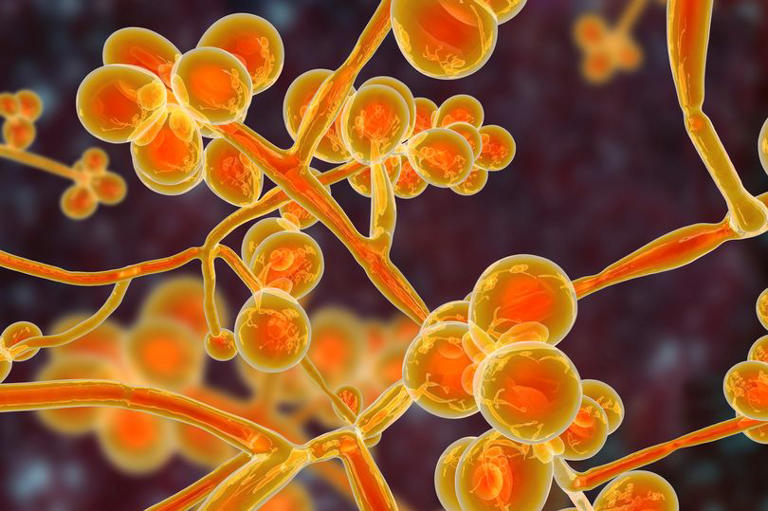
To understand the issue of COVID-19 mRNA vaccine long-term immunity, it helps to know how these vaccines work. mRNA vaccines, like the ones developed for COVID-19, instruct cells to produce a piece of the spike protein found on the surface of the SARS-CoV-2 virus. This prompts the immune system to generate a response, including the production of antibodies that can neutralize the virus if encountered in the future.
While this process is highly effective in the short term, especially in preventing severe illness, the immune system’s ability to maintain high levels of antibodies declines over time. This waning immunity has raised concerns, particularly as new variants of the virus emerge.
The Study: Why Long-Term Immunity Fades
In the recent study, researchers aimed to explore why COVID-19 mRNA vaccine long-term immunity doesn’t last as long as immunity provided by other vaccines. The study followed 19 healthy adults who received between two and five doses of COVID-19 mRNA vaccines over a period of up to three years. The goal was to determine whether the vaccines triggered the development of long-lived plasma cells, which are crucial for maintaining long-term antibody levels.
Long-lived plasma cells (LLPCs), specifically, reside in the bone marrow and can continue to produce antibodies for years, providing ongoing protection against infections. The researchers compared the presence of LLPCs specific to COVID-19 with those specific to other diseases, like tetanus and influenza.
Short-Lived Plasma Cells and Waning Antibodies
The results showed that while the COVID-19 mRNA vaccines did generate antibody-secreting cells in the bone marrow, these cells were mainly short-lived. In contrast, the immune response to tetanus and influenza involved the establishment of LLPCs, which integrated into the bone marrow’s long-lived compartments.
For COVID-19, however, the antibody-secreting cells were found primarily in short-lived compartments, meaning they did not persist in producing antibodies over an extended period. This explains why COVID-19 mRNA vaccine long-term immunity declines rapidly, with antibody levels dropping within three to six months after vaccination.
Implications for Future Vaccines
The absence of durable antibody-producing cells in the bone marrow is a key reason why the COVID-19 mRNA vaccine long-term immunity is limited. While the vaccines remain effective in preventing severe illness, their ability to prevent infections and transmission weakens as antibody levels drop. This has led to a higher incidence of breakthrough infections, particularly with the emergence of new variants.
To address this issue, researchers believe that future vaccine strategies should focus on improving the establishment of long-lived plasma cells in the bone marrow. By doing so, vaccines could provide longer-lasting immunity, reducing the need for frequent booster doses.
Comparing Immunity: COVID-19 vs. Other Vaccines
One of the key findings of the study was the difference in how the immune system responds to COVID-19 vaccines compared to other vaccines. For example, the study showed that for vaccines like tetanus and influenza, the immune system is able to generate LLPCs, leading to long-lasting immunity. These vaccines integrate antibody-secreting cells into the bone marrow’s long-lived compartments, allowing them to continue producing antibodies for years.
In contrast, COVID-19 mRNA vaccine long-term immunity does not benefit from this same mechanism. The immune system does not generate LLPCs for the SARS-CoV-2 spike protein, meaning that antibody levels decline relatively quickly. This highlights the need for new vaccine formulations or strategies that can enhance the body’s ability to produce long-lived plasma cells for COVID-19.
The Role of T-Cell Immunity
It’s important to note that while antibody levels drop, COVID-19 mRNA vaccine long-term immunity is not entirely lost. The vaccines also generate T-cell-mediated immunity, which plays a critical role in protecting against severe disease. T-cells help the immune system recognize and destroy infected cells, and this type of immunity appears to last longer than antibody-mediated immunity.
However, T-cell immunity alone is not enough to prevent all infections. Boosting both T-cell responses and antibody responses is essential for providing comprehensive protection, especially as new variants of the virus continue to emerge.
What’s Next for COVID-19 Vaccines?
The findings of this study point to the need for improved vaccine strategies that can enhance COVID-19 mRNA vaccine long-term immunity. One possible approach is developing vaccines that better mimic natural infection, which tends to generate more robust and longer-lasting immune responses. Another option is to explore adjuvants, substances added to vaccines to boost the immune response, specifically targeting the generation of LLPCs.
Researchers are also investigating different vaccine platforms, such as protein-based vaccines, that might be more effective at generating long-lived plasma cells. These next-generation vaccines could help provide more durable immunity, reducing the need for frequent booster doses and offering better protection against emerging variants.
Conclusion: Improving Vaccine Durability
In conclusion, the study highlights a crucial limitation of current mRNA vaccines: their inability to establish long-lived plasma cells in the bone marrow, which is vital for maintaining long-term antibody levels. As a result, COVID-19 mRNA vaccine long-term immunity is shorter than expected, with antibody levels dropping significantly within months after vaccination.
To overcome this challenge, future vaccine development must focus on strategies that enhance the formation of long-lived plasma cells, ensuring more durable immunity against COVID-19. While the current vaccines are effective in reducing severe illness, improving their ability to prevent infections and transmission will be key in controlling the spread of the virus in the long term.
The path forward lies in improving the durability of vaccines to offer more robust and lasting protection for global populations.
Related:
Marburg Virus Outbreak Rwanda 2024: 8 Fatal Cases Spark Dire Warnings