Early Viral Activity and Long COVID: Key Insights from Recent Research
Early Viral Activity and Long COVID: A recent study highlights how early viral dynamics and immune responses influence the development of post-acute sequelae of SARS-CoV-2 infection (PASC). This blog explores the findings and their implications for understanding and managing long COVID.
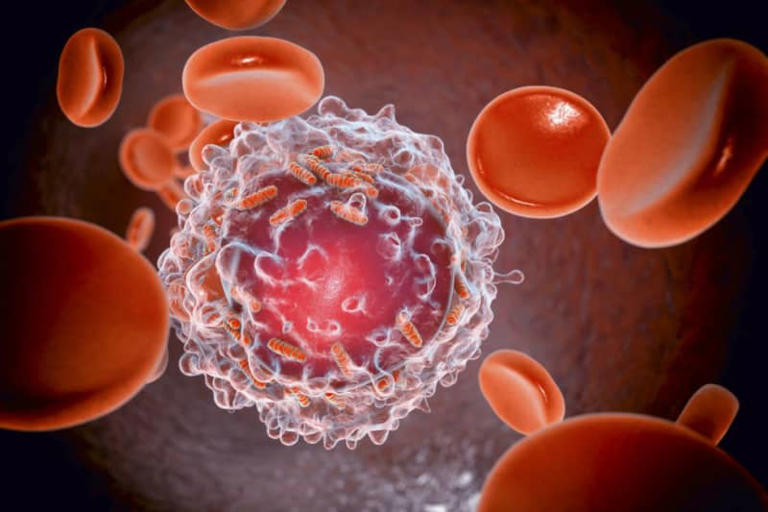
Study: Early biological markers of post-acute sequelae of SARS-CoV-2 infection . Image Credit: Starshaker/Shutterstock.com
Early Viral Activity and Long COVID
Early Viral Activity and Long COVID have become a critical area of research as scientists strive to understand why some people experience lingering symptoms long after their initial COVID-19 infection. A recent study published in Nature Communications provides valuable insights into how early viral dynamics and the body’s immune responses might play a role in developing post-acute sequelae of SARS-CoV-2 infection (PASC).
Background on Long COVID
Long COVID, or PASC, refers to a range of symptoms that persist or develop after the acute phase of a SARS-CoV-2 infection has resolved. These symptoms can include fatigue, memory issues, and difficulty breathing, among others. Despite extensive research, the exact causes of PASC remain unclear. Some studies suggest that individuals with PASC might still have SARS-CoV-2 antigens in their blood or subgenomic RNA in their tissues months after infection. Additionally, elevated levels of inflammatory markers have been observed in these patients for up to a year.
However, most research has focused on short-term outcomes, especially among hospitalized patients. This leaves a gap in our understanding of what happens during the early post-acute period and how it relates to the development of long COVID.
About the Study
To address this gap, researchers conducted a detailed study involving a cohort of individuals diagnosed with COVID-19 in San Francisco between September 2020 and May 2022. Their goal was to investigate whether early biological markers during the acute phase of infection could predict the development of PASC.
The study included 136 participants who were enrolled within five days of receiving a positive SARS-CoV-2 PCR test. Researchers collected up to 21 nasal specimens from each participant in the first four weeks following symptom onset. They also gathered questionnaires and serum samples at various intervals, including at baseline, nine days, two weeks, three weeks, four weeks, four months, and eight months after symptoms began. This data helped them assess sociodemographic characteristics, medical history, COVID-19 symptoms, SARS-CoV-2 vaccinations, and overall quality of life.
Study Methods
The researchers focused on identifying PASC by looking for COVID-19-related symptoms two to six months after the acute infection. They compared viral biomarkers and host immunological markers between those who developed PASC and those who fully recovered.
Viral Markers: The study analyzed various viral markers, including the duration and quantity of nasal SARS-CoV-2 RNA, the infectious viral load, and serum N-antigen levels.
Host Immunological Markers: The researchers also examined immune responses by measuring levels of interleukin-6 (IL-6), IL-10, tumor necrosis factor-alpha (TNF-α), interferon-alpha (IFN-α), interferon-gamma (IFN-γ), membrane cofactor protein (MCP), IFN-γ.
Quantitative and real-time reverse transcription PCR were used to assess SARS-CoV-2 RNA levels in nasal specimens. Additionally, the presence of SARS-CoV-2 was confirmed by evaluating cytopathic effects in Vero cells expressing human angiotensin-converting enzyme 2 (hACE2) and transmembrane serine protease 2 (TMPRSS2). The study employed logistic regressions and generalized estimating equations (GEE) for statistical analysis, with sensitivity analyses conducted to account for multiple comparisons.
Study Results
Among the 104 participants who were followed up, 32 (31%) developed PASC. These individuals experienced a median of 12 symptoms during their acute illness and continued to report an average of two symptoms two to six months after the initial infection.
Viral Load and Antigen Levels: Those who developed PASC showed significantly higher levels of nasal viral RNA and serum N-antigen compared to those who fully recovered. Specifically, PASC was linked to higher nasal SARS-CoV-2 RNA positivity and shedding during the first four weeks after symptom onset, as well as lower anti-spike IgG levels within the first nine days of illness.
Antibody Responses: Although the initial differences in spike IgG levels between those with and without PASC were evident, they diminished by four weeks. By then, both groups had similar levels of spike IgG. Unvaccinated individuals saw an increase in anti-SARS-CoV-2 receptor-binding domain (RBD) IgG titers over the four weeks following symptom onset.
Host Immunological Markers: The study found no significant differences in host immunological markers between those who developed PASC and those who did not. Sensitivity analyses confirmed these results.
Conclusion
The study highlights the crucial role of early viral activity and immune responses in the development of long COVID. Key findings suggest that higher viral RNA and N-antigen levels, as well as delayed antibody responses, may contribute to the persistence of symptoms. These early biological markers could be part of a broader chain of events that influence the pathogenesis of PASC.
Further research is needed to deepen our understanding of these early phases of COVID-19 and develop strategies to prevent or treat long COVID. By focusing on early indicators, we may find new ways to manage and potentially mitigate the long-term impacts of the virus.
Related:
Brain Decision Delay: Are You Living a Half-Second in the Past?