Hypervirulent Klebsiella pneumoniae Outbreak: 5 Devastating Facts You Must Know
Table of Contents
ToggleHypervirulent Klebsiella pneumoniae Outbreak: A Growing Global Health Threat
Hypervirulent Klebsiella pneumoniae outbreak poses a significant global health threat due to its antibiotic resistance and potential to cause severe illness.
Introduction
Hypervirulent Klebsiella pneumoniae outbreak is causing alarm across the globe. This deadly bacteria, resistant to many antibiotics, has been detected in 16 countries, including the UK. The World Health Organization (WHO) has raised concerns about this pathogen, which has the potential to spark the next pandemic.
Countries Affected by Hypervirulent Klebsiella pneumoniae Outbreak
The hypervirulent Klebsiella pneumoniae outbreak has been reported in the UK, US, Algeria, Argentina, Australia, Canada, Cambodia, China, India, Iran, Japan, Oman, Papua New Guinea, Philippines, Switzerland, and Thailand. Among these, 12 countries, including the UK, have reported a specific strain that has become resistant to all antibiotics used to treat it.
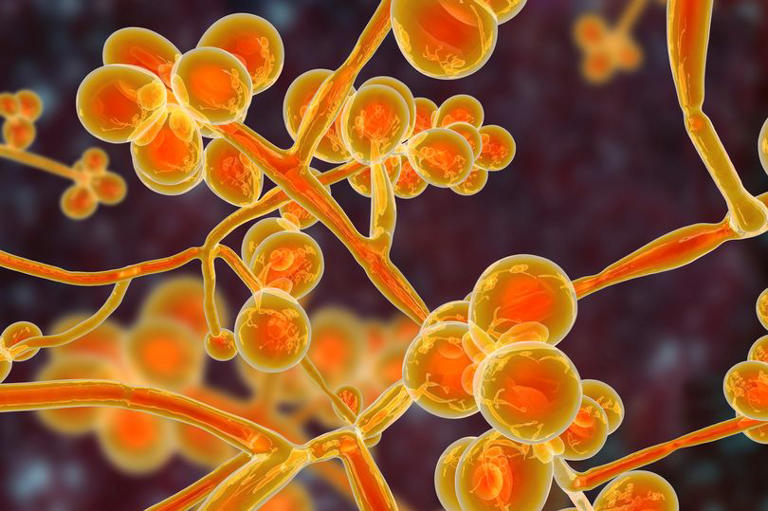
Dangers of the hvKp ST23 Strain
The hypervirulent strain, known as hvKp, particularly the sub-strain hvKp ST23, has become resistant to last-line antibiotics called carbapenems. These powerful antibiotics are typically the final treatment option when other medications fail. The increasing resistance to these critical drugs means that healthcare professionals often have no choice but to support patients while their bodies try to fight off the infection on their own.
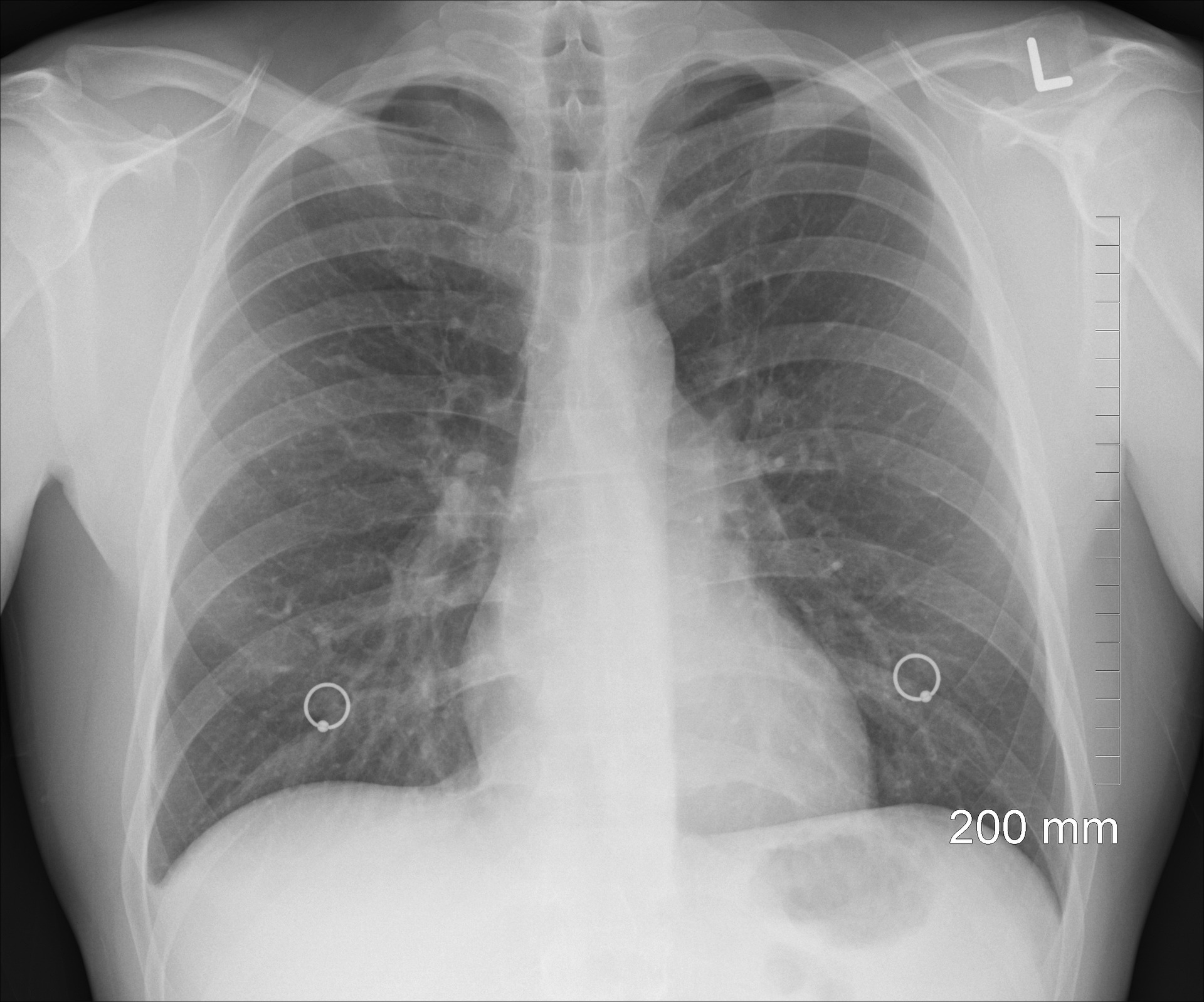
Health Impact of Hypervirulent Klebsiella pneumoniae Outbreak
It is responsible for a significant portion of pneumonia cases acquired in hospitals. This bacteria can also cause serious health issues such as urinary tract infections, meningitis, and sepsis. Despite the identified cases in over a dozen countries, the actual global spread of these strains may be greater due to insufficient testing and reporting.
WHO Recommendations and Concerns
The WHO report highlights the urgent need to enhance laboratory diagnostic capabilities to better track cases of the hypervirulent Klebsiella pneumoniae outbreak. Improved diagnostics would help identify and analyze the genetic makeup of these strains, aiding in understanding and combating their ability to infect people and resist treatment. Additionally, UK health officials have reported a troubling increase in the resistance of Klebsiella pneumoniae to frontline antibiotics, from 13.5% in 2018 to 17.4% in recent years.
Broader Context of Antibiotic Resistance
Antibiotic resistance is a growing global health crisis, often driven by the overuse and misuse of antibiotics. Without immediate action, we may face a ‘post-antibiotic’ era, where common infections become deadly. The development of new antibiotics has stalled, with only one or two new drugs introduced in the last 30 years due to the high cost and low expected revenue from these medications.
Global Impact and Future Outlook
Antimicrobial resistance (AMR) already causes significant mortality, with an estimated 1.2 million deaths annually, surpassing deaths from HIV and malaria. If not addressed, this threat could result in even higher mortality rates, with projections of 10 million deaths per year by 2050. The lack of new antibiotics and the overuse of existing ones in both medical and agricultural settings exacerbate the problem, potentially leading to a scenario where routine surgeries and treatments become extremely risky.
Economic and Medical Implications
The cost of developing a new antibiotic is estimated at £1 billion, but the revenue is predicted to be around £35 million a year. This low revenue is because health authorities will use these drugs only as a last resort to prevent new resistance from developing. Innovative funding models, such as a subscription model that pays companies for access to these drugs annually regardless of use, have been suggested but have yet to be implemented effectively.
Conclusion
The hypervirulent Klebsiella pneumoniae outbreak is a clear signal of the urgent need for global action to combat antibiotic resistance. Strengthening diagnostic capabilities, developing new antibiotics, and implementing better antibiotic stewardship are crucial steps to prevent a future where once-treatable infections become life-threatening pandemics. The WHO’s warning underscores the ongoing battle against superbugs and the importance of proactive measures to safeguard global health. By addressing this issue head-on, we can hope to avoid a future where the hypervirulent Klebsiella pneumoniae outbreak and other similar threats cause widespread devastation.
ALSO READ:
New Covid Symptoms Summer 2024: 5 Alarming Signs You Can’t Ignore